Primitive Neuro-Ectodermal Tumors (PNET) Diagnosis and Treatment
PNETs are primary central nervous system (CNS) tumors. This means they begin in the brain or spinal cord. PNET is a term that stands for a group of tumors, and these tumors are currently being reclassified and given other specific names based on their molecular features.
To get an accurate diagnosis, a piece of tumor tissue will be removed during surgery, if possible. A neuropathologist should then review the tumor tissue.
What are the grades of PNETs?
Primary CNS tumors are graded based on the tumor location, tumor type, extent of tumor spread, genetic findings, the patient’s age, and tumor remaining after surgery, if surgery is possible.
The group of tumors, formerly known as PNETs, are Grade IV tumors. This means they are malignant (cancerous) and fast-growing. These are tumor types that belong to this group:
- Medulloepithelioma
- CNS neuroblastoma
- CNS ganglioneuroblastoma
- Embryonal tumor with multilayered rosettes and other unspecified embryonal tumors
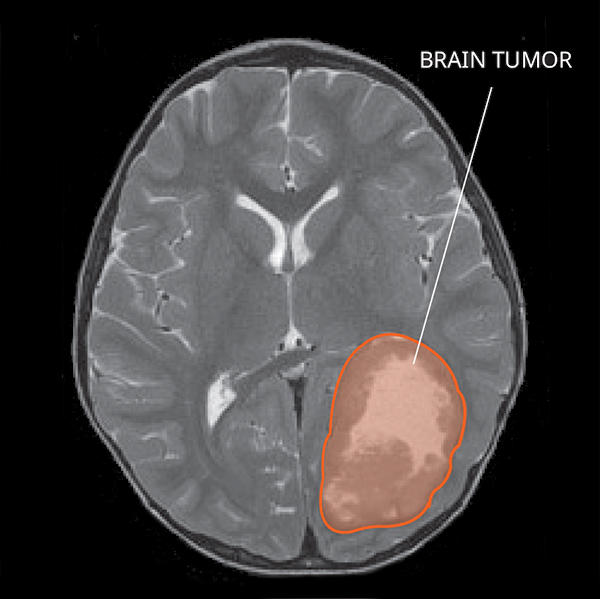
What do PNETs look like on an MRI?
PNETs usually initially appear as a single mass in the cortex, the outer layer of the brain. PNETs often enhance with contrast and more than one tumor can be identified. Sometimes, there are cysts or fluid collections found within the mass. PNETs may also have some swelling around them.
What causes PNETs?
Cancer is a genetic disease – that is, cancer is caused by certain changes to genes that control the way our cells function. Genes may be mutated (changed) in many types of cancer, which can increase the growth and spread of cancer cells. The cause of PNETs is not known. Some PNETs are related to genetic changes.
Where do PNETs form?
PNETs are commonly found in the brain and rarely, in the brainstem or spinal cord. PNETs is a group of tumors that form from the ectoderm, the outermost layer of cells of an embryo in early development.
Do PNETs spread?
PNETs can spread to other areas of the CNS and organs. When first diagnosed, about one-third of patients’ tumors have spread.
What are the possible symptoms of PNETs?
Symptoms related to PNETs depend on the tumor’s location. Here are some possible symptoms that can occur.
PNET Symptoms
- Headaches
- Seizures
- Thinking or memory problems
- Weakness
- Numbness
- Problems with balance and movement
People with PNETs in the spine may have:
- Bowel or bladder incontinence
- Pain in the back and legs
Who is diagnosed with PNETs?
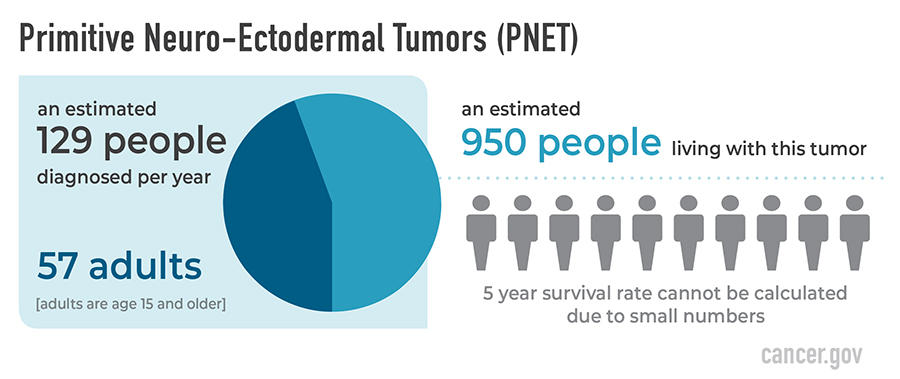
PNETs occur more commonly in children, but can occur in adults. PNETs are very rare tumors, and their classification is evolving. PNETs occur more often in males than females. They are most common in white people. An estimated 950 people are living with this tumor in the United States.
What is the prognosis of PNETs?
The likely outcome of the disease or chance of recovery is called prognosis.
PNET Prognosis
The relative 5-year survival rate for PNETs cannot be calculated due to small numbers. Many factors can affect prognosis. This includes the tumor grade and type, traits of the cancer, the person’s age and health when diagnosed, and how they respond to treatment. If you want to understand your prognosis, talk to your doctor.
What are the treatment options for PNETs?
The first treatment for PNETs is surgery, if possible. The goal of surgery is to obtain tissue to determine the tumor type and to remove as much tumor as possible without causing more symptoms for the person.
People with PNETs usually receive further treatments. Treatments may include radiation, chemotherapy, or clinical trials. Surgery is usually followed by radiation in patients 3 years old or older, sometimes including the brain and the spine. Clinical trials, with new chemotherapy, targeted therapy, or immunotherapy drugs, may also be available and can be a possible treatment option. Treatments are decided by the patient’s healthcare team based on the patient’s age, remaining tumor after surgery, tumor type, and tumor location.
Open Clinical Studies for PNETs
- Outcomes and Risk Project for Patients with Rare CNS Cancers
- Evaluation of the Natural History and Specimen Banking for Patients with CNS Cancers
- Virtual Reality Study for Patients with Brain Cancer
- Sleep Observation Study for Patients with Brain Cancer
- CALM Therapy Intervention Study for Patients with Brain Cancer
- Immune Checkpoint Inhibitor Nivolumab for Patients with Rare CNS Cancers
- ONC206 for Patients with Rare CNS Neoplasms
Learn More
- Collaborating Globally to Impact Outcomes for Rare Brain and Spine Cancers
- Four-time PNET Survivor Shares Coping Tips
- Living with a Brain or Spine Tumor

Did anyone contact you at all about Tuesday?
ReplyDeleteI gave my attorney an idea, but you would need to agree to it. That asshole put your name on it; so that leaves you in charge too.
ReplyDeleteI gave you power of attorney forms, but did that Janitor-in-a-can give them to you? (The "Cop with a mop" as my friend calls him) he was always taking out your mail away from you.
ReplyDeleteWho IS he to you, anyway?
ReplyDeleteI remember him saying to me, "he likes you better than me, but I've known him longer!" He stuck his tongue out at me in court, why don't you sic HER on HIM? LET HER TERRORIZE HIM! After lying about me in court, that put me in jail, HE DESERVES IT! He is such an immature, little baby, but emotionally, so is she!!
ReplyDelete(The command given to a dog, “sic 'em,” derives from the word “seek.”)