Hi cutie, just wanted to say hi! I am still working on paperwork. I am frazzled and hungry.
I am anticipating getting the "thing" going! My life has become complicated. Just want to see you!
Hi cutie, just wanted to say hi! I am still working on paperwork. I am frazzled and hungry.
I am anticipating getting the "thing" going! My life has become complicated. Just want to see you!
Getting business stuff done. I really feel out of the loop. Plus working on the other stuff too.
I have a good feeling about the other stuff. There are things to do, people to see and places to
go. :-)💃💪😏😏😚
Hope your day is going well!
Have a lovely day! 🌄🌞
I have you in my heart and mind! (as always!)
Be very well! Things are being done & worked out!
(As far as I hope!)
Stay positive! I am trying too! ⌣😼
You are beautiful! 🏥
Some days I feel so lonely and without purpose. One sweet appearance of light and caring can brighten up my entire outlook for a long moment in time. I feel I need to stop looking for that as my escape from my sadness and emptiness, but that thought leaves me feeling such a sense of despair that it pervades my soul with such phenomenal darkness I am certain light will never return. You are that light.
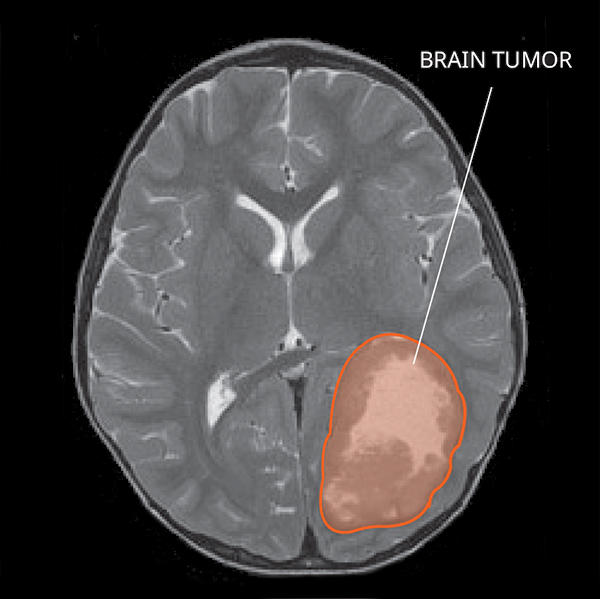
MRI of a Primitive Neuro-Ectodermal Tumor (PNET) in the brain.
PNETs are primary central nervous system (CNS) tumors. This means they begin in the brain or spinal cord. PNET is a term that stands for a group of tumors, and these tumors are currently being reclassified and given other specific names based on their molecular features.
To get an accurate diagnosis, a piece of tumor tissue will be removed during surgery, if possible. A neuropathologist should then review the tumor tissue.
Primary CNS tumors are graded based on the tumor location, tumor type, extent of tumor spread, genetic findings, the patient’s age, and tumor remaining after surgery, if surgery is possible.
The group of tumors, formerly known as PNETs, are Grade IV tumors. This means they are malignant (cancerous) and fast-growing. These are tumor types that belong to this group:
PNETs usually initially appear as a single mass in the cortex, the outer layer of the brain. PNETs often enhance with contrast and more than one tumor can be identified. Sometimes, there are cysts or fluid collections found within the mass. PNETs may also have some swelling around them.
Cancer is a genetic disease – that is, cancer is caused by certain changes to genes that control the way our cells function. Genes may be mutated (changed) in many types of cancer, which can increase the growth and spread of cancer cells. The cause of PNETs is not known. Some PNETs are related to genetic changes.
PNETs are commonly found in the brain and rarely, in the brainstem or spinal cord. PNETs is a group of tumors that form from the ectoderm, the outermost layer of cells of an embryo in early development.
PNETs can spread to other areas of the CNS and organs. When first diagnosed, about one-third of patients’ tumors have spread.
Symptoms related to PNETs depend on the tumor’s location. Here are some possible symptoms that can occur.
People with PNETs in the spine may have:
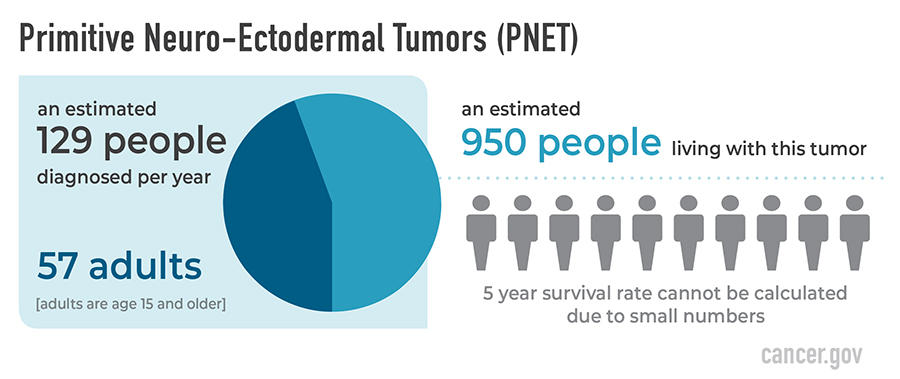
PNETs occur more commonly in children, but can occur in adults. PNETs are very rare tumors, and their classification is evolving. PNETs occur more often in males than females. They are most common in white people. An estimated 950 people are living with this tumor in the United States.
The likely outcome of the disease or chance of recovery is called prognosis.
The relative 5-year survival rate for PNETs cannot be calculated due to small numbers. Many factors can affect prognosis. This includes the tumor grade and type, traits of the cancer, the person’s age and health when diagnosed, and how they respond to treatment. If you want to understand your prognosis, talk to your doctor.
The first treatment for PNETs is surgery, if possible. The goal of surgery is to obtain tissue to determine the tumor type and to remove as much tumor as possible without causing more symptoms for the person.
People with PNETs usually receive further treatments. Treatments may include radiation, chemotherapy, or clinical trials. Surgery is usually followed by radiation in patients 3 years old or older, sometimes including the brain and the spine. Clinical trials, with new chemotherapy, targeted therapy, or immunotherapy drugs, may also be available and can be a possible treatment option. Treatments are decided by the patient’s healthcare team based on the patient’s age, remaining tumor after surgery, tumor type, and tumor location.